Why am I obsessed with blood glucose?
I am obsessed with blood glucose because there is no better easily observed predictor of overall health, longevity, and well-being.
My husband has been passionate about low carb nutrition for diabetics and for over all good health since the early 90s. At this time, the medical community was still in the throes of the low fat hypothesis. People thought my husband was something of a nut–and I can remember heated fights at dinner parties where other physicians accused my husband of medical malpractice for encouraging low carb diets. Things have started to turn around.
You’ll notice the call to sanity implicit to the article linked above. People might ask, if low carb treatment of diabetics is so glaringly superior to any pharmaceutical or nutritional approach available, why does it still not reach the level of mainstream? Because the burden of evidence placed upon it is almost impossible to achieve. Meanwhile, clinicians such as the ones listed as the authors of the above study, continue to use it with success. Their patients lives are more important. You can’t argue with the results once you put it into practice. Especially those of us who have to put it into practice ourselves.
After we were married in 2000, while we were living in Manhattan, he would take the train to Dr. Richard Bernstein’s office and Dr. Bernstein kindly let my husband shadow him. Dr. Bernstein is one of the doctors listed in the article above and he is the pioneer patron saint of low carb nutrition. His first big splash was when he revolutionized diabetes management in the 70s as the inventor of continuous blood glucose monitoring. Billions have been made on this radical idea in diabetes management as the test strips and the glucometers still fly off the shelves. But they left the accompanying nutritional philosophy in the dust.
Despite being ridiculed and mocked, Dr. Bernstein continued with low carb management of diabetes. Not just his patients. Dr. Bernstein himself is a Type 1 who, prior to discovering he could control his own diabetes by reducing carbohydrates, was headed for an early death. This is what I call SKIN IN THE GAME, people. So many nutritional and health gurus are people who started off lean, fit, healthy, and beautiful. The ones I listen to are ones with SKIN IN THE GAME. These are the people who risk their own health on what they are preaching at high stakes. Fake tans and poseur sympathy with the obese and health challenged is not what I call skin.
My husband had read Dr. Bernstein’s book, Dr. Bernstein’s Diabetes Solution: The Complete Guide to Achieving Normal Blood Sugars
but seeing him in action was a different experience altogether. Bernstein’s results with diabetics–both Type 1 and Type 2–were hard to argue with. My husband began encouraging his patients to use Dr. Bernstein’s nutritional protocol to treat diabetes. He was convinced (and still is) that Type 2 diabetes is a curable disease, given the right nutritional approach.
It was challenging, however. People need a lot of training and a lot of support to change their entire point of view on diet and food. It is a new way of eating, a new way of thinking about their diabetes, and a new way of living. Most of you probably understand without much explanation, contemporary primary care medicine is not really set up for this kind of lifestyle change. Moreover, more frequently PCPs like my husband (who’s specialty is internal medicine) tend to see diabetes as an endocrinologist’s problem. My husband didn’t see it that way. Then, he saw his job as keeping you out of the hospital and getting you out quickly if you had to go in. He knew that this mission hinged on getting his patients the best control of their blood sugar they could get. And he knew that was all nutritional.
That’s why we started the nutrition clinic. I did the coaching and patient education and he saw them for in-office visits to check on their products through blood work and physical exam. The already good results he had in his practice became staggering. Patients went from 7 or 8 medications to 1 or 2, or even none. We sought many ways to find a way to better integrate the clinic into the existing group practice he had, but to no avail. We are still working on it.
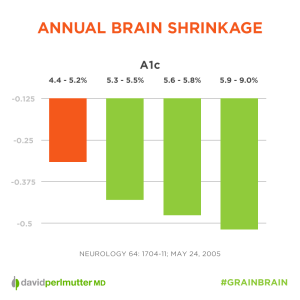
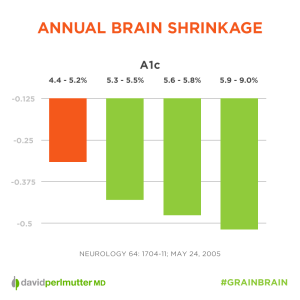
For his board re-certification, we both worked together to collate a much larger data set to include his entire practice, not just the patients in the clinic. Data doesn’t lie: all complications associated with diabetes were directly correlated to HbA1c, and that the lab reference ranges were set too high. We saw complications starting at much lower threshold than what the reference ranges indicated. The lower the A1C, the less problems. Period.
This isn’t controversial, per se. Few in medicine would argue with this correlation. What may be contentious is our current standard, in line with Dr. Bernstein’s—an HbA1c below 5. What may be more contentious still is that we don’t consider diabetics a special case. In America we are essentially all diabetic because of the high carbohydrate, pro-inflammatory diet that has become standard. Therefore the reference ranges labs provide are drawn from population studies done on populations that are already on a path to multiple disease processes, neurodegeneration, and premature aging. The average ranges are above what you want to be shooting for.
This makes the doctor’s evaluation of your HbA1c at 5.2 as “normal” suspect. To us, you are already pre-diabetic.
It turns out that we are not alone in our point of view.
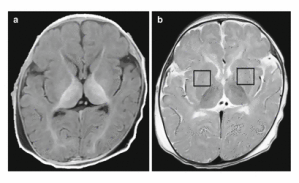
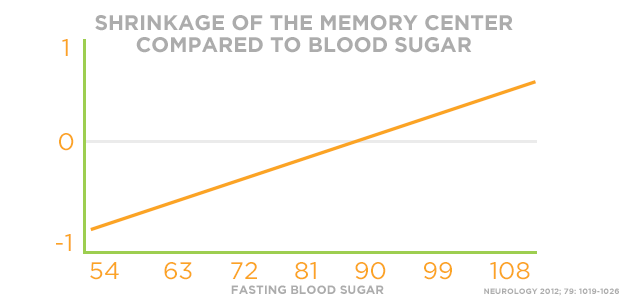
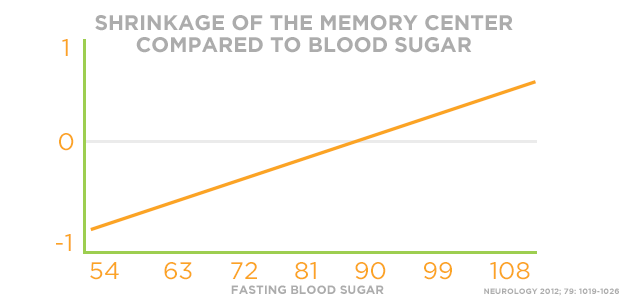
Dr. Perlmutter, author of Grain Brain: The Surprising Truth about Wheat, Carbs, and Sugar–Your Brain’s Silent Killers , recently posted a German study that correlated A1C and fasting glucose with lower memory and reduced hippocampal structure. In other words, the higher your A1C, the smaller your brain.
, recently posted a German study that correlated A1C and fasting glucose with lower memory and reduced hippocampal structure. In other words, the higher your A1C, the smaller your brain.
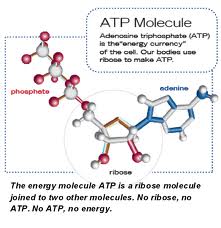
What is the key to managing those sugars, according to Dr. Perlmutter? Not just low carb. HIGH FAT.
This isn’t the only correlation. It isn’t a coincidence that the place at which there is negative shrinkage–that is to say GROWTH–is the same place that Dr. Seyfried, author of Cancer as a Metabolic Disease: On the Origin, Management, and Prevention of Cancer finds tumors shrinking and cancer being de-fanged.
finds tumors shrinking and cancer being de-fanged.
There are other places where our lower level numbers are justified. For one small example, in April of last year, Nature published an article that showed that hyperglycemia was associated with multiple kinds of cancer development. And “evidence is also provided that risk is already increased in the pre-diabetic and normal ranges for several cancers.”
If you haven’t already read it, my post on defining keto-adaptation with low blood sugar (and HbA1C), explains why I think that defining keto-adaptation without at least a measure of fasting blood glucose is meaningless. The above provides further justification for the levels we set.
Have you bought your glucometer yet?