http://blogs.plos.org/obesitypanacea/2014/05/26/scienceoffat/
Ketosis is Neuroprotective. Full stop.

As has become more frequent, the study cited below is trying to mimic the neuroprotective quality of ketones with pharmacological agents. The maxim to “follow the money” is hard to ignore–in this case one needs only to look at the amount of studies being done to find a pharmacological agent that can mimic what ketones do in the brain to understand just how therapeutic what I call “neuroketosis” is. In short: folks know there would be money to be made if we can put ketosis in a pill.
In the paleosphere, an argument rages about whether maintaining continual nutritional ketosis—which is different than both starvation ketosis and diabetic ketoacidosis in form and effect—is optimal or even desirable. Primarily, there is a tendency to overlook the brain because people think of it as separate from the body–and the Paleo movement, like Western culture in general, is driven by body obsession in large part. There is also a tendency to think the value of ketosis only applies to diseased brains, not understanding that “neuroprotective” means preventative as well as therapeutic.
The general discussion also fails to understand that “neuroprotective” is not brain specific: when we talk about neuroprotection we are talking about the entire CNS and the HPA-axis that resides in the brain, and therefore the endocrine system. We are still steeped in the Cartesian dualism that separated brain from body. That the brain IS the body and is networked as part of a complex system doesn’t seem to compute.
If you have this form of mind-blindness you can partition the neuroprotective part out of the conversation. The conversation therein derived is then driven more by the path of least resistance than what might be optimal for health, well-being, and longevity. (And what will get you into your skinny jeans.) It would be great if it was neither optimal nor desirable to be in continual ketosis. Maintaining nutritional ketosis in our culture and with our childhood habits is difficult. It requires constant vigilance. I wish it could be easier. For some of us with metabolic damage, cocktail sauce with shrimp cocktail can knock you out of ketosis and take a day or two to re-enter. I wish I could say “hey you gotta live.”
It is never easy to buck the entire culture or your personal bioculture which, if you were raised in the standard western diet, is built on a deranged metabolism. As any opiate addict will tell you, your neurological addictions to extremes of excitation and oblivion are never easy to combat.
We also start the conversation with a common confirmation bias: eating shouldn’t be so difficult and complicated. If it is “natural” we shouldn’t have to fight so hard and it shouldn’t be difficult. The fact is that it should be natural. It should be easy. It isn’t in today’s world where thousands of businesses are competing for your attention and appetite. It is definitely more difficult to maintain ketosis within a metabolic context that has become dependent on the neurological effects of glycolysis for feelings of pleasure, relaxation, and stimulation. There is a neurology of addiction at work. The more information on ketones and the brain become available the more we know this is true.
In the study of epistemology–the science of knowledge itself–we know that at certain points, we arrive at what we call a paradigm shift. A paradigm shift rarely (if ever) occurs with a single study that demonstrates something in a settled way. It comes when we approach a critical mass of information. In order to understand how the neurology of ketosis (and glycolysis) works we have to understand how it controls even the way we read data. If our current eating habits are satisfying certain neurological addictions, the law of confirmation bias will make us reject what might make us change our habits. If our habits precluded steady ketone production we might start to doubt that ketones are really that important.
The neuroprotective quality of ketone bodies is at that tipping point that I’ve described above in the sense of a Kuhnian paradigm shift. The studies are so small and specialized one might miss it, however. There is no doubt that what I am going to call neuroketone production is optimal for neurological function and neural longevity. So as I have written elsewhere the question of maintaining a metabolic state that encourages the brain to use ketones instead of glucose or lactate is not “should we?” But “why shouldn’t we?”
In this conversation—one that starts from the assumption that neuroprotection is KEY–the questions that plague us: nuts? Dairy? Calories? Cycling? Are very simple.
What are your ketones doing?
In all honesty, there are other questions. Nutritional status and inflammatory markers for sure. But the fundamental question must be are you making—and preferentially using—ketones?
Funny enough: if you aren’t asking this question you may end up having to pay 500 bucks a month to buy a manufactured agent that mimics their function.
The brain is key.
via Nutritional or pharmacological activation of HCA2 ameliorates neuro… – PubMed – NCBI.
New Study Explains How Low-Carb Diet Reduces Inflammation
Compare this to white adipocytes which actually produce cytokines–so much so that recent research has led to the neologism “adipokines” to describe the rheumatologic implications of an abundant white fat layer.
Stored white adipose layer behaves in exactly the opposite way that MOBILIZED fat does.
The Well-Formulated Ketogenic Diet

Over the course of the next week I am going to describe the pillars of our program one at time. We can help our clients through the program with customization and offer problem-solving and support. We enjoy the work and provide value. Really, however, it is easy to follow the program on your own. Soon, we will have a book available with sample meal-plans and more thorough information as well as case studies, but I will cover the basics right here for you for free. Free is the new money right? 🙂 Stay tuned.
- Sleep Training.
- 3-6 cups of leafy greens, sulfur, and colorful vegetables served and prepared with quality fats.
- A balanced fatty acid profile.
- Adequate protein.
- Stress Management.
- Increasing Oxygen.
- Sunlight.
Top 3 Keto Mistakes (And How to Correct Them)
1. Too Much Protein
Many “ketogenic diets” advocate a higher protein approach. Higher protein approaches are valid for weight loss but they aren’t classically “ketogenic” in that they aren’t promoting maximal ketone production and ketone metabolism. How do we know? Because in clinical applications of the ketogenic diet, anything below the classic ketogenic ratio the optimal therapeutic value of the ketogenic diet ceases (and we would argue it ceases being truly ketogenic.)
No one really knows for sure why the ketogenic diet is therapeutic for so many metabolic diseases including cancer, some strains of Alzheimer’s disease, Parkinson’s, and autoimmune disorders. There are several proposed mechanisms of action including increased mitochondrial function and biogenesis, the suppression of lactate, inherent properties in beta-hydroxy butyrate, improved astrocyte metabolism, and others. Whatever the case, there is some kind of unidentified, therapeutic “magic” in ketogenesis, and we believe that we shouldn’t just aim for weight loss but for maximal disease prevention.
Disease states are just normal physiological processes that have traveled too far in one direction or another. One might say that we are all more or less along the spectrum of metabolic disease simply by living the American lifestyle. So what is therapeutic is not just for those who are in active, progressive disease states, but for all those who seek improved health and disease prevention.
Having established this: “making ketones” is not the same thing as making ketones and using them optimally. Why is this important? Because KetoChix don’t care just about their skinny jeans they care about their skinny genes. This diet functions as epigenetic therapy, which assists the treatment and prevention of diseases that most impact quality of life and mortality. Too much protein provides a glucose stream (through gluconeogenesis) that competes with the use of ketones as a preferred source of fuel. There are a lot of arguments on the internet about this and the rate at which your body converts protein to glucose is going to be different based on your current diet, your overall health, and your genetics. Both protein and fat lower blood glucose compared to carbohydrate but protein impacts blood glucose at roughly 3xs the rate of fat. Just how much protein is going to affect your blood glucose is determined by your level of insulin resistance (measured by your insulin production and waist circumference). This is why people get into such mad arguments on the internet about protein–“it doesn’t affect my blood sugar!” It’s variable based upon your state of metabolic health. This is why KetoChix test blood glucose in order to determine where their protein threshold is. What’s awesome about the ratio is that fat and protein attenuate each other. If you keep the fat higher than the protein, you may find that you are able to eat MORE protein than if you keep the protein higher than the fat. What does attenuate mean? It means that fat lessens the blood glucose impact of protein, just as both protein and fat will attenuate the impact of glucose derived from carbohydrate.
Most people who get into regular blood glucose testing learn quickly that if their protein is too high, their blood glucose moves out of the ideal ketogenic range. The range that KetoChix find in their protein again is specific to them, their size, and their level of activity but most Ketochix find that their ideal protein level lies between 6 and 12 ozs of fatty protein sources per day.
2. Not Testing Lean Body Mass and Blood Glucose
KetoChix are body hackers. The ketogenic ratio is a guideline but the method of PLAN-MEASURE-PLAN will allow you to make a custom-designed keto plan for YOU. To do this you must establish regular testing and measurement intervals. We also suggest that those measures be maximally meaningful. To start, measure blood glucose (and ketones if you wish) each morning before eating and calculate both weekly and monthly averages. (BG measures are precise but not accurate–which means there are some deviation in the measures that will equal out over averages.) Still use your daily readings as a rough guide to test what you ate the day before but keep your eye on the weekly and monthly averages.
Don’t weigh (or at least, don’t weigh and only weigh.) Measure your body with a tape measure and choose an online body fat calculator to get your approximate BODY FAT PERCENTAGE. I can’t emphasize this enough. The scale will only frustrate you because keto stimulates adrenergic activity–which means, even in the absence of exercise you will gain some lean mass. This has a tendency to make the scale go up, especially in the beginning, or to make the losses appear minimal.
3. Ignoring Step One is Sleep
Step One is Sleep. End of discussion. This is the one people rebel against the most. It requires discipline and focus, and for some people major lifestyle changes that are difficult to take on. But nothing is going to fix your cortisol levels (and therefore blood sugar dysregulation) if you don’t get the proper sleep. This is perhaps the most under-exploited weight loss strategy of all. We lose weight while we sleep. If we do not go to sleep according to how the sun moves across the sky it makes it difficult to lose weight.
Keto-Adaptation is Multi-Level
When we talk about “keto-adaptation” we seem to be talking about one process but there are really several. The HPA axis in the brain has to adapt. The muscles have to adapt. The astrocytes have to adapt. The liver has to adapt. The gut has to adapt. The adipose layer itself has to adapt. And the pancreas has to adapt. Biodiversity, genetics, disease, are all going to dictate different timelines on all of these processes. How damaged is your pancreas? How damaged is your stomach and intestinal tract? And so on. Your muscles may become quite efficient at using free fatty acids and ketones while your pancreas remains on the diabetes spectrum. It can take time for beta cells to calm down, regenerate. The complexity of these multiple processes come to the fore more completely when you look at just how complex ketogenesis is. The fact remains, the ketogenic diet works for so many things we can’t quite get a handle on the multivariate mechanisms of action in it. Most of the mechansims are not just complex, they seem, with our limited knowledge, contradictory.
Let’s take appetite control for example.
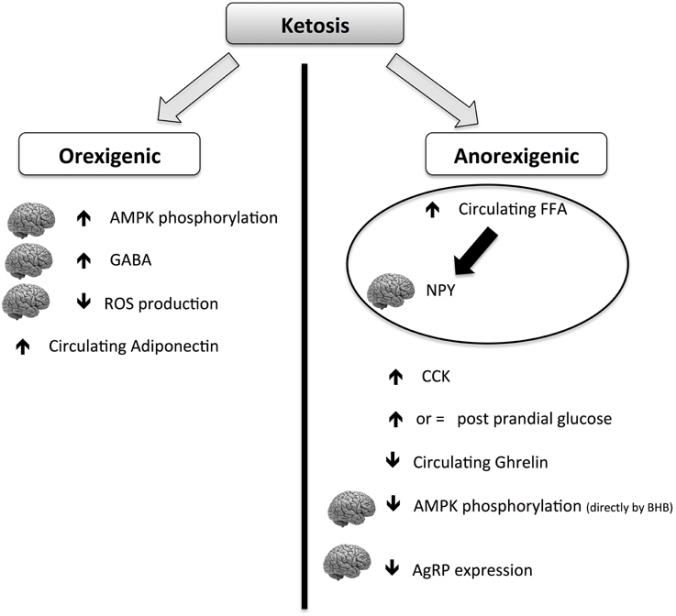
Most of us who have even dabbled in keto have experienced its appetite suppressing effects. It is part of its popularity: the reduction in appetite makes the formerly impossible task of dieting much easier to take on. It’s one thing to use will power and careful calorie counting to lose weight. It’s quite another when you suddenly have no desire to eat and can go long intervals between meals without even a second thought. It’s empowering.
Clinically, however, the hard-core scientific evidence lags behind. An interesting review of the existing literature on ketogenic diet and its food intake and appetite effects was published in February. The existing literature is sparse and low power, but what data exists supports the anecdotal experience of low appetite. However, we personally have also experienced some “fat-adapted” patients, with good blood glucose control that also experience hunger. Anecdotally, it appears on the discussion boards in the ketoverse all the time.
The above chart from the review being discussed here shows that keto diets have a paradoxical ability to cause both hunger and appetite suppression, though the net effect seems to be appetite suppression. It does seem to explain some mechanisms by which it could make some people feel MORE hungry.
Additionally,we have hypothesized that there is a tipping point in ketone production that can bring on an insulinergic effect. People commonly confuse “ketosis” with “ketoacidosis” (this is what is behind the horrified look of some health professionals when you mention you are practicing and/or prescribing the ketogenic diet–often, they don’t know the difference). DKA–diabetic ketoacidosis–only occurs in type 1 diabetics. It can occur rarely in type 2 diabetics who have progressed so far in their disease that they are now both type 1 and type 2 diabetics at the same time. It is important to understand that DKA can only occur in an extremely low or negative insulin environment because the way we regulate ketones in the body normally is through insulin release. So, think of the subject who prior to the ketogenic diet was on her way to type 2 diabetes. Her increased body mass and her constant high glucose stimulated the production of insulin producing beta cells in the pancreas. Once on keto, a high level of ketones, particularly if they are being artificially raised with excessive mct consumption, all of those beta cells go to work on lowering the ketones with surges of insulin. The pancreas does not down-regulate as quickly as the body loses fat mass and gains insulin sensitive tissues in its place. It certainly cannot down regulate as quickly as the blood glucose drops to around 85 or below on a steady basis, which happens in some keto dieters in a matter of days. In this time there might be overproduction of insulin that causes hunger, fatigue, thirst, and irritability. This will certainly adjust on its own, but there could be some interventions including increased exercise and some insulin-sensitivity inducing medications that could assist during the adaptation period. Subjects during this period may also find it difficult to lose weight and might retain water. This is part of the pancreatic adaptation period, which in those who were previously type 2 diabetic or on the road to it, may experience it. This may also occur later in the process for those subjects who were previously on diabetes meds and they are slowly withdrawn.
Returning to this review, it also thoroughly discusses other possible (likely?) mechanism for reduced food intake on the ketogenic diet including the ever popular gut biome thesis and the underexplored neuro-endocrine juncture. Of particular interest is the discussion of GABA and glutamine–because this is connected to the well-known anti-convulsant properties of the ketogenic diet (often low GABA is associated with seizure activity). No true conclusions are reached because these orexogenic and anorexigenic hormones and peptides are paradoxical. Insulin signals satiety—except when too much of it causes hunger, for example. Fascinating and maddeningly complex.
We do know, however, that the regulation of food intake is key to not just initial weight loss but maintaining that weight loss and the consequent health benefits long term. We similarly know that this regulation occurs between a lengthy conversation between the brain, adipose tissue, and the so-called “second brain” in the gut. It seems to be the cause of a lot of misunderstanding between the obese and the usually non-obese medical and health and fitness community that attempts to assist them. There is just a different conversation going on in a body that reaches a tipping point of adiposity than in one that remains below that threshold. This is key to thinking of compassionate and effective ways to help the obese.
via Ketosis, ketogenic diet and food intake control: a complex relation… – PubMed – NCBI.
Ridley Scott and Your Alien Fat Layer
Wherein ever so quietly we learn that de novo synthesis of corticosteriod and oxysterols in adipocytes creates a defense mechanism against forming new fat cells…when there is overfeeding on….a high fat diet.
The adipose layer functions like a parasite with its own endocrine and vascular system, which disrupts the host’s endocrine and cardiovascular system, ultimately the lymphatic system. I have said it before and I will say it again: obesity is an autoimmune disorder. The question is: is it a disorder? Or is it disorder-ing? That may or may not be a relevant question. For the moment, let’s think about, collectively, how the adipose layer, when grown in excess of energy storage needs, becomes like a functioning parasitic organism, an alien being, draining the host of nutrients, fostering inflammation, promoting angiogenesis, and producing hormones that disrupt the host organism’s already delicate hormonal balance.
The Ridley Scott “Alien” metaphor is only slighly hyperbolic. In a 2003 review of the “physiology of adipose, ” the authors of the study write: “it is essential to remember that adipose tissue normally operates as a structured whole” and exists in a feedback loop with the autonomic nervous system, the endocrine system and the host blood supply–it self-regulates producing its own hormonal responses and can generate additional vascularity through angiogenesis to support and grow itself. Just think about that for a minute. It’s a little John Hurt-ish, is it not?
Usually, that system works as most physiological systems do: through negative feedback. Your blood pressure rises, which in turn stimulates the baroreceptors, which signal the release of hormones that bring the blood pressure down. Negative feedback is self-regulating through something like a gas-brake system. What happens when a system is gas-gas? This is what happens in morbid obesity or “diabesity” where the system suddenly seems to move into a positive feedback mode. The fatter and lower lean mass we get, the fatter and lower lean mass we get. The question is why?
Well, it turns out that there is a negative feedback system built into the adipose layer–the fat tissue should become steroidogenic and produce steroidal hormones that signal the cell to stop creating new fat cells. It turns out this occurs most acutely in the presence of…a high cholesterol diet. If your diet is de jure or de facto low cholesterol diet all bets are off.
via De novo synthesis of steroids and oxysterols in adipocytes. – PubMed – NCBI
Ketones may Inhibit Lactate Metabolism in Astrocytes
The brass ring for pharmaceutical companies is figuring out how keto works in treating epilepsy in patients that don’t respond to drugs.
Some folks In the paleosphere aren’t interested in “diseased populations” and fail to see why an interest in fitness and weight loss should be connected to nutritional therapies used to treat disease states. It is short-sighted because disease states are always normal physiological processes gone too far in one direction or another. We therefore learn the most about normal physiology from studying disease states.
This is true of all fields of medicine. The entire field of neurology was founded on studying traumatic brain injuries in WW I veterans. By studying what happens when particular parts of the brain are injured we learn, in part, how the brain functions when it is whole. The famous case of Phineas Gage, for example, not only impacted the field of neurology, it has created an entire paradigm shift in certain branches of philosophy as his symptomology challenged our Cartesian notions about the division between reason and emotion and ultimately body and mind.
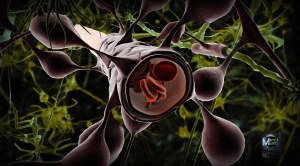
A compound that inhibits lactate metabolism in astrocytes seems to imitate keto. Astrocytes make lactate but they also make ketones. If lactate metabolism plays a role in epilepsy what happens when the body isn’t making BHB, the natural lactate suppressant?
One doesn’t have to look far to understand the role of astrocytic lactate metabolism and rapid neuronal aging.
Now who might be interested in diets that are therapeutic in epilepsy?
KetoChix Lift Up Heavy Things and Put Them Down Again
A recent study from the University of Sydney suggests that resistance training has a direct impact on age-related cognitive decline. As I’ve said elsewhere you can’t talk about the body without talking about the brain. When you talk about the brain you imply a conversation about the body; when you talk about the body you imply a conversation about the brain.
Further, we have developed simple testing measures for mitochondrial function that involve an improvement in V02 max–and while you can achieve v02 max improvement nutritionally, the most expedient way to do it is through exercise.
Interesting to note in this study—they used what they call “sham” measures–creating fake cognitive testing and fake exercise routines so the subjects wouldn’t know what exactly was being tested. Seated calisthenic and mildly aerobic measures did not work. It was specifically resistance training that improved all measures of cognitive function tested in the study.
KetoChix are Brainy Chix. We Lift Heavy Things and Put Them Down Again.
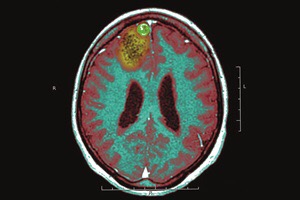
Ketones and the Blood-Brain Barrier
Often people will ask me where we get our definition of keto-adaptation as being consistent blood glucose below 85 and morning ketones between.5 and 3. It’s an obvious logical step in understanding how the body adapts. Ketones and glucose compete for fuel. You can’t get into a zero glucose state–there are brain cells, for example, that can only operate on glucose, although the amount of glucose the brain needs is minimal and doesn’t need to come from dietary sources. The brain can use multiple substrates (fuel sources) and becomes more efficient when it does so. The brain that operates only on glucose is an inefficient brain. The problem is the Standard American Diet trains brains to run on glucose only–so much so that it becomes glucose dependent and its use of other available substrates becomes minimal. This leads to premature aging, neurodegenerative disease, and flat out grey matter shrinkage. It also provides epigenetic therapy reducing the expression and/or effect of genes that lead one toward cancer, CVD, and auto-immune disorders.
You can see why we don’t give a shit about your skinny jeans. It’s usually a nice secondary effect. But it isn’t our goal.
The goal is to get our glucose dependent brains to be operating on multiple other substrates, which it really is designed to do. Astrocytes, for example, make their own ketones in the brain, it wants to be using ketones, even if we’ve beaten it into submission with years of glucose flooding. All we need to do is provide the brain with enough ketones (and pryuvate and lactate–but that’s another post) to let it begin to operate optimally.
But how do we do that? Well, people started testing ketones. If I’m making ketones then I must be using them, right? Well. Hold on there. We know that high amounts of circulating ketones and even pure fatty acids can reach the mitochondria of the muscle tissue through capillaries providing an energy source.
It’s only in considering just HOW the ketones reach the brain that the circulating blood glucose becomes not just relevant to keto-adaptation but crucial to it.
The brain is surrounded by something called the BBB–the blood brain barrier. The BBB has selective permeability that varies in different metabolic states. Those who have hung around KetoChix a bit understand that everything in biochemistry works in ratios (that’s why we figure out our food macros not in absolute calories but in ratios of fat:protein + carb) and substrates in the body have the tendency to act like a clutch and gas pedal. In this case you can think of glucose as clutch and ketones as the gas. Because the ketones can only GET to the brain if the circulating plasma glucose is low. It works in an inversely proportional ratio.
The important thing to remember is that glucose and ketones have the gas and clutch relationship. What people started doing when measuring ketones was to verify that you are eating sufficient fat and keeping carbs low enough that you are actually making them. That’s only the first step. The idea is that you are using them, preferentially. The lower your blood glucose, the more your tissues—all of your tissues not just brain tissue–are using ketones as their PREFERRED fuel. Since large population studies correlate disease states with fasting blood glucose of over 85, we can guess where that gas and clutch rhythm reaches its maximal efficiency.
Some more studies to read if you want background and like to connect dots:
http://www.ncbi.nlm.nih.gov/pubmed/7611392
http://www.ncbi.nlm.nih.gov/pubmed/3884391